Evolving Therapeutic Approaches: Beyond Traditional Talk Therapy
Mental health care is rapidly changing. We are witnessing significant advancements in how we approach healing and well-being. A critical area of focus is dual diagnosis. This is when mental health conditions co-occur with substance use disorders. This complex situation demands an integrated and compassionate treatment approach for effective recovery.
In this extensive guide, we will explore the innovative ways mental health treatment is evolving. We will dig into new therapeutic modalities and the importance of integrated care, especially in regions like East Tennessee. Personalized patient journeys and the transformative role of technology in practice management will also be discussed. Our goal is to shed light on these modern strategies, helping individuals find comprehensive support, such as that offered for mental health dual diagnosis East TN.
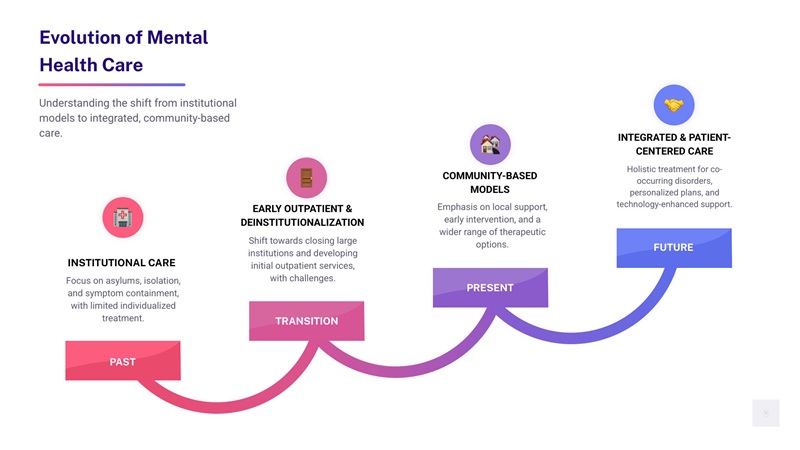
Mental health care has undergone a profound change, moving from historical institutional models to a more nuanced, community-based, and integrated approach. This evolution reflects a deeper understanding of the complexities of mental well-being and the interconnectedness of mind and body. Early interventions often focused solely on symptom management, with little attention paid to underlying causes or co-occurring conditions. However, contemporary innovations prioritize a patient-centered philosophy, recognizing each individual’s unique journey and needs. This paradigm shift emphasizes early detection, holistic treatment, and sustained recovery, ensuring that care is not just reactive but also proactive and empowering. The goal is to foster resilience and equip individuals with the tools to steer life’s challenges, ultimately leading to improved quality of life and long-term wellness.
The landscape of mental health treatment is continually enriched by the development and refinement of therapeutic approaches that extend far beyond conventional talk therapy. Modern interventions are increasingly evidence-based, meaning their effectiveness has been rigorously tested and proven through scientific research. These therapies are designed to address a wide spectrum of mental health challenges, offering targeted strategies for various conditions. For instance, Cognitive Behavioral Therapy (CBT) helps individuals identify and change negative thought patterns and behaviors, while Dialectical Behavior Therapy (DBT) focuses on emotional regulation, mindfulness, and interpersonal effectiveness. Eye Movement Desensitization and Reprocessing (EMDR) is particularly effective for trauma, helping individuals process distressing memories. Motivational Improvement Therapy (MET) assists those struggling with substance use by strengthening their motivation for change.
Beyond these well-established methods, there’s a growing appreciation for holistic therapies and experiential approaches. These modalities recognize the intricate connection between mind, body, and spirit, aiming to heal the whole person rather than just addressing symptoms. Experiential therapy, for example, uses activities like outdoor adventures or creative arts to help individuals explore emotions, build self-esteem, and develop coping skills. This blend of scientific rigor and holistic understanding represents a significant innovation in mental health care, ensuring that individuals receive comprehensive and custom support. Understanding the role of therapy in addiction recovery is crucial for anyone seeking help, as it forms the cornerstone of lasting change.

Common Evidence-Based Therapies & The Conditions They Treat:
- Cognitive Behavioral Therapy (CBT): Depression, anxiety disorders, PTSD, substance use disorders.
- Dialectical Behavior Therapy (DBT): Borderline Personality Disorder, emotional dysregulation, chronic suicidality, substance use disorders.
- Eye Movement Desensitization and Reprocessing (EMDR): Post-Traumatic Stress Disorder (PTSD), other trauma-related conditions.
- Motivational Improvement Therapy (MET): Substance use disorders, encouraging internal motivation for change.
- Acceptance and Commitment Therapy (ACT): Anxiety, depression, chronic pain, substance use disorders.
- Interpersonal Therapy (IPT): Depression, focusing on interpersonal relationships and social roles.
- Psychodynamic Therapy: Explores unconscious patterns and past experiences influencing present behavior.
The Growth Of Specialized, Evidence-Based Modalities
The evolution of mental health treatment has led to a proliferation of specialized, evidence-based modalities, each designed to address specific aspects of mental well-being. Trauma-informed care, for instance, has become a cornerstone of modern practice, recognizing the pervasive impact of trauma on mental health and ensuring that services are delivered in a way that avoids re-traumatization. Techniques like Somatic Experiencing help individuals release trauma stored in the body, while Neurofeedback trains the brain to regulate its own activity, improving focus, mood, and sleep.
Furthermore, personalized medicine is beginning to make inroads into psychiatry. This involves tailoring treatment plans based on an individual’s unique biological and genetic makeup. Genetic testing in psychiatry, though still in its early stages, holds promise for predicting how a person might respond to certain medications, reducing the trial-and-error often associated with prescribing. A deeper understanding of neurobiology, as explored by researchers like Koob & Volkow (2016) in their neurocircuitry analysis of addiction, continues to inform these advancements, allowing us to target the brain mechanisms underlying various conditions more precisely. These innovations underscore a move towards more precise, effective, and individualized care.
Integrating Holistic & Experiential Therapies
Alongside scientific advancements, there’s a growing recognition of the profound impact of the mind-body connection on overall health. Integrating holistic and experiential therapies into treatment plans provides a comprehensive approach to healing. Practices like yoga in recovery promote physical well-being, reduce stress, and foster mindfulness, helping individuals connect with their bodies and emotions in a healthy way. Art therapy offers a non-verbal outlet for expression, allowing individuals to process complex feelings and experiences that might be difficult to articulate verbally.
Equine-assisted therapy involves interacting with horses to develop trust, communication skills, and emotional regulation. Mindfulness and meditation techniques teach individuals to be present, observe their thoughts without judgment, and cultivate inner peace, which are invaluable skills for managing stress and preventing relapse. These therapies complement traditional approaches by fostering self-findy, building resilience, and promoting a sense of well-being that extends beyond symptom reduction. They are integral to comprehensive addiction treatment and mental health support, helping individuals develop a richer, more balanced life.
The Rise Of Integrated Care: A Mental Health Innovation For Complex Needs
One of the most significant innovations in mental health treatment is the rise of integrated care, particularly for individuals facing co-occurring disorders, often referred to as dual diagnosis. A dual diagnosis disorder refers to a co-occurring mental condition and substance use disorder. This means an individual is simultaneously battling both a mental health illness (such as depression, anxiety, PTSD, or bipolar disorder) and a substance use disorder (involving alcohol, illicit drugs, or prescription medications). This complex interplay means that each condition can exacerbate the other, creating a challenging cycle of self-medication, worsening symptoms, and increased risk of relapse.
For example, someone with anxiety might use alcohol to calm their nerves, which over time can lead to alcohol dependence and worsen their underlying anxiety. Conversely, prolonged substance abuse can trigger or intensify mental health symptoms. The National Institute on Drug Abuse (NIDA) highlights common comorbidities with substance use disorders, underscoring the prevalence of this issue. An estimated half of those battling addiction also suffer from at least one mental health disorder. This statistic alone emphasizes why integrated treatment is not just beneficial, but essential. Without it, individuals are often caught in a revolving door of treatment, addressing one condition only to have the other trigger a relapse. Integrated care seeks to break this cycle by treating both conditions simultaneously and holistically.
Why Integrated Treatment Is Crucial
Integrated treatment is crucial because it treats the whole person, recognizing that mental health and substance use disorders are deeply intertwined and cannot be effectively addressed in isolation. When these conditions are treated concurrently, by the same team of professionals, individuals experience coordinated care that leads to significantly improved outcomes. Research consistently shows that those who do not treat these conditions at the same time are twice as likely to experience a relapse within six months of leaving treatment. This stark statistic underscores the importance of a unified approach.
The Substance Abuse and Mental Health Services Administration (SAMHSA) advocates for integrated treatment for co-occurring disorders, providing evidence-based practices (EBP) kits to guide effective implementation. This approach ensures that treatment plans are comprehensive, addressing both the psychological and physiological aspects of each condition. It helps individuals develop healthier coping mechanisms, understand the triggers for both their mental health symptoms and substance use, and build a strong foundation for long-term recovery. These integrated models are becoming more common, with specialized programs like those for Mental health dual diagnosis East TN demonstrating how targeted, localized care can address complex needs. By fostering collaboration among therapists, psychiatrists, and addiction specialists, integrated care offers a path to genuine healing and sustainable well-being.
A New Frontier For Mental Health Innovation: Co-Occurring Disorders
Addressing co-occurring disorders represents a new frontier for mental health innovation, challenging traditional systemic approaches that often treated mental health and addiction in separate silos. Breaking down these silos is critical because the interaction between mental health disorders and substance abuse is complex and bidirectional. For instance, the most common mental health disorders, depression and anxiety, frequently co-occur with substance use. Blanco et al. (2012) highlighted differences among major depressive disorder with and without co-occurring substance use disorders, emphasizing the distinct treatment considerations required.
Substance abuse and mental health conditions can both be caused by genetics, stress, and trauma, further complicating diagnosis and treatment. This necessitates collaborative care models where interdisciplinary teams work together to develop a single, comprehensive treatment plan. This integrated approach not only improves patient outcomes but also streamlines the care process, making it more efficient and less fragmented. The 2022 National Survey on Drug Use and Health from SAMHSA provides key indicators of substance use and mental health in the United States, further underscoring the widespread need for such integrated solutions. By understanding and addressing the intricate relationship between mental health and addiction, we can pave the way for more effective and compassionate care.
Personalizing The Patient Journey Through A Continuum Of Care
A hallmark of modern mental health innovation is the commitment to a client-centered approach, ensuring that each patient’s journey is personalized and supported through a comprehensive continuum of care. This means recognizing that there’s no one-size-fits-all solution for recovery. Instead, treatment plans are individualized, carefully crafted to match the specific needs, goals, and circumstances of each person. This often involves a stepped-care model, where the intensity of treatment is adjusted as the individual progresses, ensuring they receive the right level of support at every stage. From initial assessment to long-term aftercare planning, the focus remains on empowering the patient and fostering their autonomy.
The continuum of care acknowledges that recovery is a dynamic process, not a linear one. It provides a flexible framework that can adapt to an individual’s changing needs, allowing for seamless transitions between different levels of care. This holistic perspective ensures that individuals are not abruptly discharged once acute symptoms subside but rather are guided towards sustainable recovery through ongoing support and resources. This personalized approach to treatment, whether through comprehensive addiction treatment or specific mental health programs, is vital for fostering lasting change.
Table: Comparing Levels Of Care For Dual Diagnosis Treatment
Feature Inpatient/Residential Partial Hospitalization Program (PHP) Intensive Outpatient Program (IOP) Hours per Week 24/7 supervision and structured activities 5-8 hours/day, 5 days/week (day treatment) 3-5 hours/day, 3-5 days/week (less intensive than PHP) Living Situation Resides at the treatment facility Lives at home or in a sober living environment Lives at home or in a sober living environment Level of Support Highest level of medical and therapeutic support High level of structured therapy, some medical oversight Moderate level of structured therapy and support Ideal For Acute crisis, severe symptoms, needing detox, unstable Stepping down from inpatient, needing significant structure but not 24/7 care, stable living environment Stepping down from PHP, needing structured support while maintaining work/school, strong support system Focus Stabilization, intensive therapy, medication management Transition, skill-building, therapy, relapse prevention Maintaining recovery, integrating skills, community reintegration Understanding Different Levels of Care
The continuum of care is built upon various levels of treatment, each designed to meet specific needs and provide appropriate support. Inpatient stabilization, often the initial step for individuals in acute crisis or requiring medical detoxification, provides 24/7 supervision and intensive therapeutic intervention. This is followed by Partial Hospitalization Programs (PHP), which offer a structured day treatment environment. In a PHP, individuals attend therapy sessions for several hours a day, typically five days a week, but return home or to a sober living facility in the evenings. This level of care is ideal for those who need significant structure and support but do not require round-the-clock medical supervision.
As individuals progress, they may transition to an Intensive Outpatient Program (IOP). IOPs provide a more flexible schedule, with therapy sessions typically held for a few hours a day, three to five days a week. This allows individuals to maintain their work, school, or family commitments while still receiving crucial therapeutic support. Finally, traditional outpatient services offer the lowest level of intensity, providing ongoing therapy and support as individuals fully reintegrate into their daily lives. The goal of this seamless transition between levels is to ensure sustained recovery, as highlighted in discussions comparing IOP vs. PHP and outpatient vs. inpatient rehab.
The Future Of Treatment: A Focus On Mental Health Innovation
The future of treatment is firmly rooted in a continuous focus on mental health innovation, particularly in the field of long-term recovery and community integration. This involves developing customized aftercare plans that are as unique as the initial treatment plans. These plans are not merely a list of recommendations but a dynamic roadmap for sustained recovery support, incorporating elements like ongoing individual psychotherapy and group therapy.
A key innovation is the increasing role of peer support specialists – individuals who have lived experience with mental health and substance use disorders and can offer invaluable guidance and empathy. Family involvement and education are also being recognized as critical components, as a supportive home environment significantly contributes to long-term success. Furthermore, community integration initiatives help individuals rebuild their lives, connect with resources, and establish healthy social networks. Programs like PHP and IOP are pivotal in bridging the gap between intensive treatment and independent living, ensuring that individuals have the tools and support necessary to thrive long after formal treatment concludes.
Technology’s Role In Modernizing Practice Management & Access To Care
Technology is revolutionizing mental health care, making it more accessible, efficient, and patient-centered. The digital change sweeping across healthcare has profoundly impacted practice management and how individuals access support. Telehealth platforms, for instance, have become indispensable, allowing individuals to connect with therapists and psychiatrists from the comfort of their homes, breaking down geographical barriers and increasing convenience. Virtual therapy sessions maintain the efficacy of in-person care while offering flexibility that was once unimaginable.
Electronic Health Records (EHRs) have streamlined administrative processes, ensuring that patient information is securely stored, easily accessible to authorized providers, and can be shared seamlessly across different care settings. This reduces paperwork, minimizes errors, and allows clinicians to spend more time focusing on patient care. Furthermore, patient engagement tools, such as secure messaging portals and online appointment scheduling, empower individuals to take a more active role in their treatment journey. This technological integration is not just about convenience; it’s about fundamentally changing how mental health services are delivered and managed, making quality care more attainable for everyone.
Enhancing Accessibility & Engagement
One of the most profound impacts of technology in mental health is its ability to improve accessibility and engagement, particularly for underserved populations or those in remote areas. Telehealth platforms have effectively broken down geographical barriers, allowing individuals in rural East Tennessee, for example, to access specialized care that might not be available locally. Mental health apps provide immediate support, offering tools for mindfulness, mood tracking, and coping strategies directly on a smartphone. These apps can serve as valuable adjuncts to traditional therapy or as initial resources for those hesitant to seek formal treatment.
Digital support groups offer a safe and anonymous space for individuals to connect with peers, share experiences, and receive encouragement. Online assessment tools can help individuals identify potential mental health concerns early, guiding them towards appropriate professional help. Even wearable technology is beginning to play a role, monitoring biometrics and activity levels that can be correlated with mood and sleep patterns, providing valuable data for both patients and clinicians. This technological accept is making mental health support more proactive and integrated into daily life.
Streamlining The Administrative Side Of Care
Beyond direct patient care, technology is significantly streamlining the administrative side of mental health practice management, making operations more efficient and reducing the burden on providers. Online insurance verification systems simplify the often-complex process of determining coverage, allowing patients to quickly understand their financial responsibilities and preventing unexpected costs. A simplified admissions process, often facilitated by online forms and digital communication, makes it easier for individuals to begin treatment, removing potential barriers that could delay access to care.
Digital aftercare resources, such as online portals with educational materials, relapse prevention plans, and community resource directories, ensure that support continues long after formal treatment ends. Data-driven treatment adjustments, enabled by EHRs and other tracking tools, allow clinicians to monitor patient progress more effectively and make informed decisions about care plans. Practice management software integrates scheduling, billing, and clinical documentation, freeing up valuable time for mental health professionals to focus on what matters most: providing high-quality, compassionate care. This operational efficiency ultimately translates into better patient experiences and outcomes.
Frequently Asked Questions About Innovations In Mental Health
What is dual diagnosis and why is it important to treat it?
Dual diagnosis, often referred to as co-occurring disorders, is the simultaneous presence of a mental health condition (like depression, anxiety, or PTSD) and a substance use disorder. It’s crucial to treat both conditions simultaneously because they often influence and exacerbate each other. For example, individuals might use substances to self-medicate mental health symptoms, which can lead to addiction and worsen their mental state. Untreated, dual diagnosis significantly increases the risk of relapse, worsens overall health outcomes, and makes long-term recovery much more challenging. Integrated treatment, addressing both conditions concurrently, is proven to be the most effective approach for sustainable healing.
What makes dual diagnosis treatment different from traditional addiction treatment?
Traditional addiction treatment often focuses primarily on substance cessation and relapse prevention, sometimes overlooking underlying mental health issues. Dual diagnosis treatment, however, is fundamentally integrated. It recognizes that mental health and substance use disorders are interconnected and must be treated together by the same clinical team. This means a comprehensive treatment plan that addresses both the psychological symptoms of the mental health disorder and the behavioral patterns of substance use. Therapies are custom to manage both conditions, and medication management may be used for mental health symptoms alongside addiction recovery strategies. This holistic approach leads to more stable and lasting recovery.
What are the benefits of seeking treatment at a dual diagnosis center in East Tennessee?
Seeking treatment at a dual diagnosis center in East Tennessee offers several key benefits. First, these centers specialize in integrated care, providing expert treatment for both mental health and substance use disorders simultaneously, which significantly improves recovery outcomes and reduces relapse risk. Second, local centers offer the advantage of proximity, allowing individuals to remain closer to their support systems, family, and community resources during and after treatment. This local focus also means staff may have a deeper understanding of regional challenges and resources. Finally, these centers often provide a continuum of care, from inpatient to outpatient programs, ensuring that individuals receive the appropriate level of support as they progress through their recovery journey.
Conclusion
The field of mental health is undergoing a remarkable period of innovation, driven by a deeper understanding of complex conditions like dual diagnosis and a commitment to patient-centered care. We’ve explored how evolving therapeutic approaches, from specialized evidence-based modalities to integrated holistic practices, are offering more effective paths to healing. The rise of integrated care models, particularly for co-occurring disorders, represents a pivotal shift, recognizing the interconnectedness of mental health and substance use and underscoring the critical need to treat the whole person.
Furthermore, the personalization of the patient journey through a comprehensive continuum of care ensures that individuals receive custom support at every stage of recovery, from intensive inpatient programs to flexible outpatient services and robust aftercare. Finally, technology is playing an increasingly vital role, enhancing accessibility, streamlining administrative processes, and empowering both patients and providers. These innovations collectively paint a hopeful picture for the future of mental health treatment and practice management, promising more effective, compassionate, and accessible care for all who seek it.
